Edema (swelling) and Phlebolyphedema
Edema (swelling) and Phlebolyphedema
Leg, calf, foot, or ankle swelling?
 Alsara Vein Clinic has helped many patients achieve relief from Edema.
Alsara Vein Clinic has helped many patients achieve relief from Edema.
Edema (swelling) of the calf, ankle, foot, or leg is a common symptom of varicose veins that allows blood to flow backward and pool in the legs. Over time, some blood and other fluids can leak out of the vein into the surrounding tissue causing Edema (swelling). Edema Specialist and Vein Specialist Dr. Sam Gupta can help diagnose and treat Edema (swelling). Dr. Gupta is certified by the American Board of Venous and Lymphatic Medicine.
At Alsara Vein Clinic, we treat vein problems all day, every day.
Call us at 816-396-0245 for a Consultation

Leg, calf, foot, or ankle swelling (Edema) is a common sign of varicose veins.
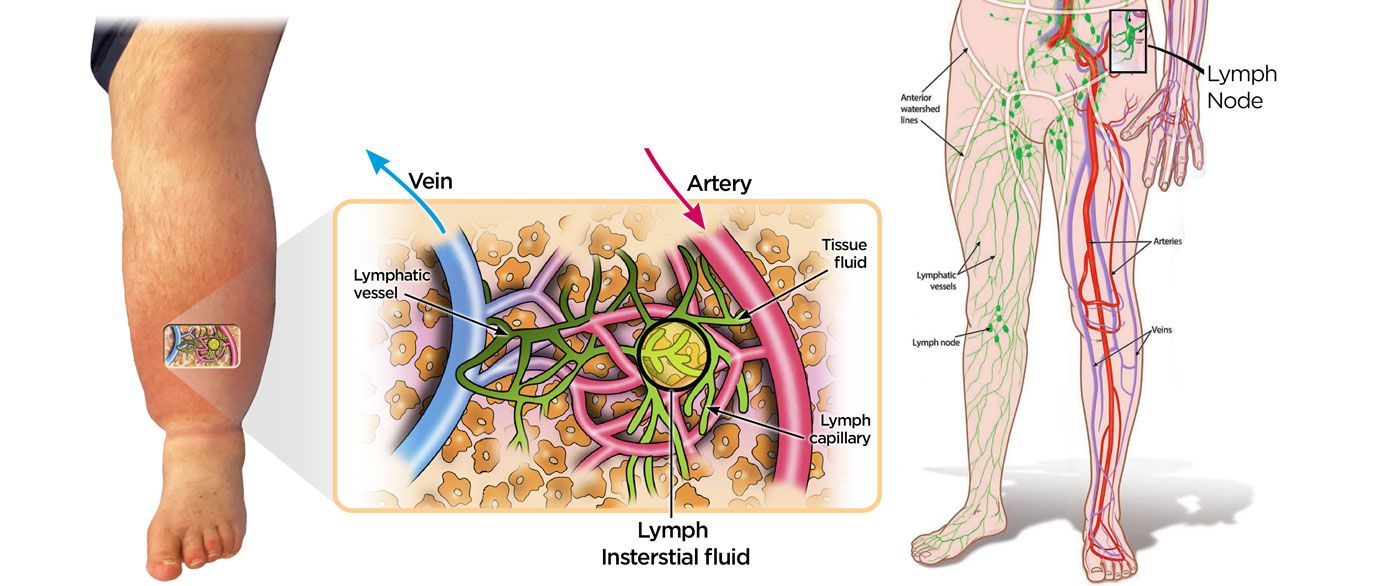
The normal flow of blood in leg veins is against the force of gravity; from the foot to the thigh and then up towards the heart. When veins are stretched and enlarged (become varicose), they are too weak to overcome the force of gravity causing the blood to flow backward and pool in the legs. As the pooling continues throughout the day, the pressure inside the vein walls continues to increase. Eventually, some blood and other fluids can leak out of the vein into the surrounding tissue.
 The pooling of blood, increased pressure and subsequent “leakage” causes swelling in the ankles and feet as gravity pulls the fluid down. As leakage continues, swelling can also be noted in the lower calf region and extend to the knee or even the thighs.
The pooling of blood, increased pressure and subsequent “leakage” causes swelling in the ankles and feet as gravity pulls the fluid down. As leakage continues, swelling can also be noted in the lower calf region and extend to the knee or even the thighs.
Swelling is more noticeable at the end of the day, especially if you have spent much of it sitting or standing still. When you elevate your legs, for example when you are sleeping, gravity is no longer a force working against the flow of the blood in your leg veins hence swelling is reduced. However, when you sit or stand, the swelling recurs. Other factors that can contribute to increased swelling include lifting or straining, pregnancy, heat (such as hot baths or sauna), and hormonal changes (that further relax and stretch the weak veins).
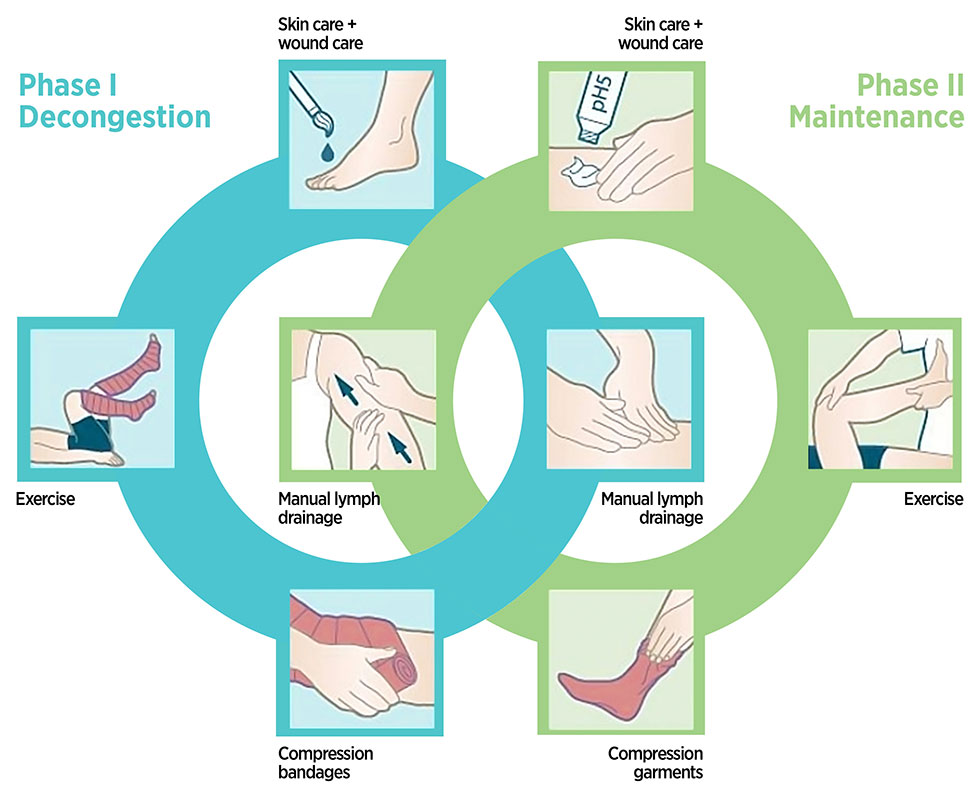
 During the initial stages of edema, graduated compression stockings may be enough to diminish the tendency of the veins to stretch and control edema. Over time, patients may notice increasing leg fatigue, swelling, thinning of the skin, and discoloration of the overlying skin. Complications such as painful blood clots in the vein, bleeding from veins close to the skin surface, and nonhealing leg sores may develop. Many patients may also notice unsightly spider and varicose veins (Corona Phlebectatica).
During the initial stages of edema, graduated compression stockings may be enough to diminish the tendency of the veins to stretch and control edema. Over time, patients may notice increasing leg fatigue, swelling, thinning of the skin, and discoloration of the overlying skin. Complications such as painful blood clots in the vein, bleeding from veins close to the skin surface, and nonhealing leg sores may develop. Many patients may also notice unsightly spider and varicose veins (Corona Phlebectatica).
Because of the potentially serious and long-term complications of varicose veins, proper treatment is important, and the best results are obtained before complications have already developed. A Vein Specialist can use a Duplex Ultrasound to check “leaky” varicose veins and treatment options.
Varicose Vein Treatments are coved by insurance including Medicare and Medicaid