Many patients now recognize that varicose veins may not be visible from the outside. Most of our patients report experiencing tiredness, cramping (charley horse), restlessness, or swelling in the legs. Those whose condition has not reached one of the advanced stages often wonder if they are at increased risk of anything that could be limb or life-threatening.
At least one-third of our patients clearly have signs of advanced venous insufficiency – when varicose veins have progressed to a point where the chronic pooling of blood (stasis) in the legs causes skin changes. They may notice skin discoloration, thickening or hardening of the skin, recurrent skin infections, bleeding that can be profuse, and poorly healing sores in the legs. In addition, varicose veins may be an early warning sign of potentially deadly blood clots.
We routinely see patients with blood clots. Some are referred by their primary care providers and others present themselves with concerns about blood clots. Yet there are many patients who are surprised to find that they have a blood clot when we examine them using duplex ultrasound.
Introduction
Restless Leg Syndrome (RLS) is characterized by an irresistible urge to move the legs to alleviate discomfort, ranging from aching and throbbing to itching and crawling sensations.2 Articulating these sensations can be challenging for some patients.
Who gets it?
Initially documented in 1945, RLS, also known as Willis-Ekbom disease3, was reported to affect around 5% of the population. Recent studies, however, indicate a prevalence ranging from 3% to 15%. It tends to occur more frequently in women, with a nearly 2:1 female-to-male ratio. As age advances, there is a positive correlation with RLS prevalence. Genetics plays a role, as up to 25% of first-degree relatives of individuals with RLS report similar symptoms.4
Connecting Varicose Veins and RLS
Even in the 1940s, when Restless Leg Syndrome (RLS) was first identified, Dr. Ekbom suggested that venous disease could be a potential cause. However, it took around fifty years to firmly establish this connection. A groundbreaking 1995 study published in the Journal of Dermatologic Surgery treated 113 individuals with restless legs and ultrasound-confirmed vein disease using sclerotherapy.5 Surprisingly, 98% of participants reported immediate relief. Subsequent studies have consistently supported this link, uncovering RLS symptoms in individuals with primary and recurrent varicose veins1. Addressing superficial venous insufficiency has proven effective in alleviating RLS symptoms for most patients. Nonetheless, it's essential to acknowledge that certain conditions, including iron deficiency anemia, pregnancy, kidney failure, various neurological conditions, and specific medications, can also contribute to RLS symptoms.
Explaining the connection
Impaired venous blood return in the legs, particularly in chronic venous insufficiency (CVI), may drive the subconscious urge to move the legs (RLS), forcing you to use your muscles that help pump blood back to the heart. Inflammation associated with CVI could lead to overactive nerves, intensifying the situation. Nighttime leg cramps and pain, often linked to varicose veins, can further disrupt sleep, aggravating leg restlessness.
Determining if Varicose Veins might be responsible for Restless Legs
A straightforward and noninvasive duplex ultrasound in your Vein Specialist’s office can identify any underlying venous issues. The Vein Specialist will review a treatment strategy if venous insufficiency is found. Typically, the affected veins are closed using one of the FDA-approved treatment modalities to reroute blood flow through healthier veins.6
Conclusion
Restless Leg Syndrome (RLS) is a common issue often linked to varicose veins. You might also be encountering other symptoms of varicose veins and associated venous insufficiency, including sensations of heaviness, fatigue, aching, cramping, and swelling in the legs. If left untreated, the condition can worsen, leading to potential complications such as blood clots, bleeding, frequent skin infections, and slow-healing sores. Medications for RLS, such as Ropinirole and Pramipexole, may mask the symptoms without addressing the underlying problem. Reach out to Alsara Vein Clinic at 816-396-0245 for a complimentary Consultation.
Take the initial step towards relief and an improved quality of life.
- Restless legs syndrome symptoms in primary care: a prevalence study. Nichols DA, Allen RP, Grauke JH, et al. Arch Intern Med. 2003;163:2323–2329
- Restless legs syndrome: diagnostic criteria, special considerations, and epidemiology:Sleep Med. 2003;4:101–119.
- Restless legs syndrome/Willis-Ekbom disease diagnostic criteria Sleep Med. 2014;15:860–873. [
- Treatment of Leg Veins for Restless Leg Syndrome: A Retrospective Review, Swaminathan et al, Cureus 2019
- The effect of sclerotherapy on restless legs syndrome Dermatol Surg 1995 April 21
- The effect of endovenous laser ablation on restless legs syndrome Hayes et al Phlebology June 2008
 There are also reports of blood clots in patients with COVID-19 who are at home and staying active. Swelling in the legs is the most common sign of blood clots. Some patients with COVID-19 develop a condition called “Covid toes” – red, swollen toes that may be due to small clots in the blood vessels of the feet.
There are also reports of blood clots in patients with COVID-19 who are at home and staying active. Swelling in the legs is the most common sign of blood clots. Some patients with COVID-19 develop a condition called “Covid toes” – red, swollen toes that may be due to small clots in the blood vessels of the feet.

 Chronic Venous Insufficiency (CVI) is a medical condition in which the veins in the legs don’t function properly, making it difficult to pump blood back to the heart. This leads to circulation problems and a variety of leg symptoms.
Chronic Venous Insufficiency (CVI) is a medical condition in which the veins in the legs don’t function properly, making it difficult to pump blood back to the heart. This leads to circulation problems and a variety of leg symptoms.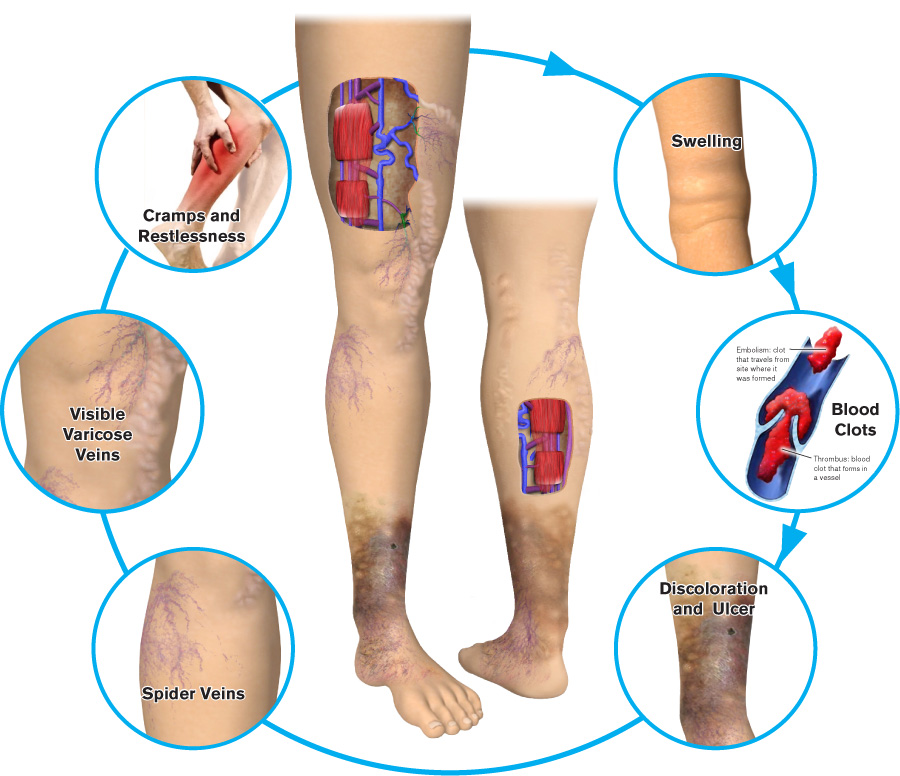



 Varicose veins increase the risk of deep vein thrombosis (DVT) by five times
Varicose veins increase the risk of deep vein thrombosis (DVT) by five times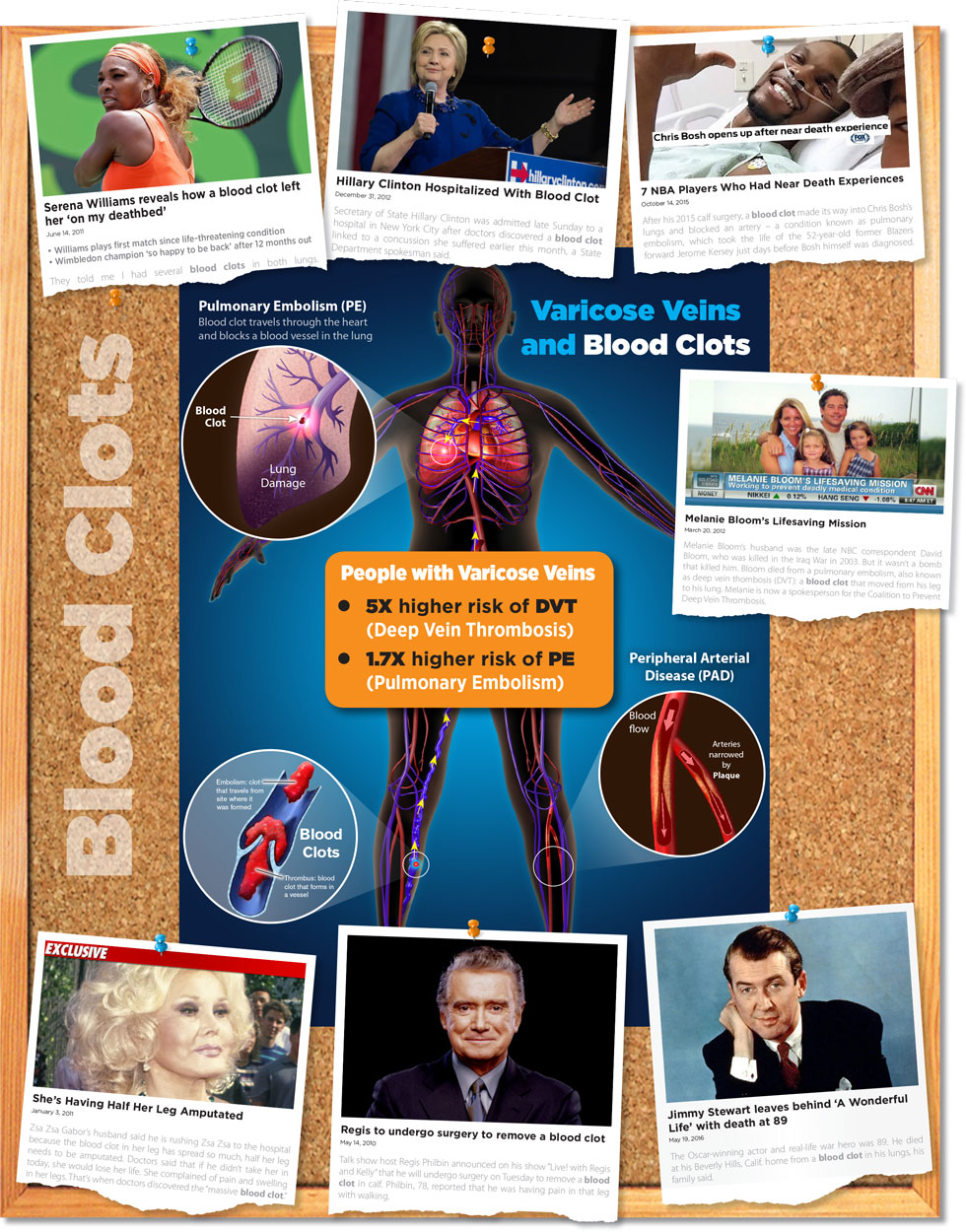

 Stay Hydrated
Stay Hydrated