My 9-year-old daughter recently had a major change in her career plans, from wanting to be a mermaid to being a Physician. I am still trying to find similarities between the two professions to better understand what led to this “slight” change in the career path for her. Some rightly said that children are like mirrors; they reflect all that they see and hear. Perhaps she sees the difference that our work has made in the lives of many including her teachers who came seeking care. I am certain that the stories of numerous patients have impacted her. For instance, hearing that several of my patients have “charley horses”, it was only natural for her to request one… “Dad, I would like one (charley horse) too!”
Although charley horse is a commonly used term for cramps in the leg, typically in the calf muscles, I was curious to learn about the origin of the term. There is a debate about the origin of the nickname. According to one source, there was a lame horse named Charley whose work was to help move things around a baseball park. The picture of the limping horse was so deeply entrenched in memories of the ballplayers that they started referring to each other as “charley horse” if they pulled a leg muscle or developed any minor impairment in their legs. Since the 1880s, the slang word lingered and is now commonly used to describe a sudden tightening or contracting sensation that lasts a few seconds to several hours and can be painful as well as debilitating.
 The dreaded charley horse is reported to affect up to 60 percent of adults who have reported the presence of nocturnal leg cramps in the form of a painful spasm, tightening of calf muscles, and twinges. Numerous causes of charley horses have been described in the medical literature including muscle fatigue, dehydration, mineral deficiency, and poor circulation (venous insufficiency).
The dreaded charley horse is reported to affect up to 60 percent of adults who have reported the presence of nocturnal leg cramps in the form of a painful spasm, tightening of calf muscles, and twinges. Numerous causes of charley horses have been described in the medical literature including muscle fatigue, dehydration, mineral deficiency, and poor circulation (venous insufficiency).
During the initial stages, it is a good idea to gently massage the affected areas and use over-the-counter pain medication such as ibuprofen.
 There are some easy ways to help prevent charley horses including staying hydrated, eating a balanced diet, avoiding excessive sugars and caffeine, and avoiding overexertion.
There are some easy ways to help prevent charley horses including staying hydrated, eating a balanced diet, avoiding excessive sugars and caffeine, and avoiding overexertion.
There are numerous old wives’ tales about home remedies from drinking pickle juice, using quinine, to the use of a bar of soap under the bedsheet to fend off charley horses. There is scarce scientific data to back these claims. One Harvard study described an ion channel called TRPV1 that activates the spinal column and inhibits the firing of nerves to dull the pain of cramps. It is possible that the protons in pickle juice use this mechanism to help alleviate the discomfort. Remember that a mere 2 ounce shot of the juice may contain a few hundred milligrams of sodium, so anyone with heart disease, hypertension, or renal insufficiency should exercise caution. Quinine has potential side effects such as severe bleeding and heart arrhythmias. There does not seem to be any harm from using a bar of nice smelling soap if you have a strong urge to try it under your bedsheet. If nothing else, it will help your bed smell nice!
Having a magnesium, potassium, or calcium deficiency can contribute to leg cramps, however, your medical history must be taken into account before you consider using any over-the-counter supplements. It is always better to discuss with your Primary Care Provider to avoid any adverse interactions.
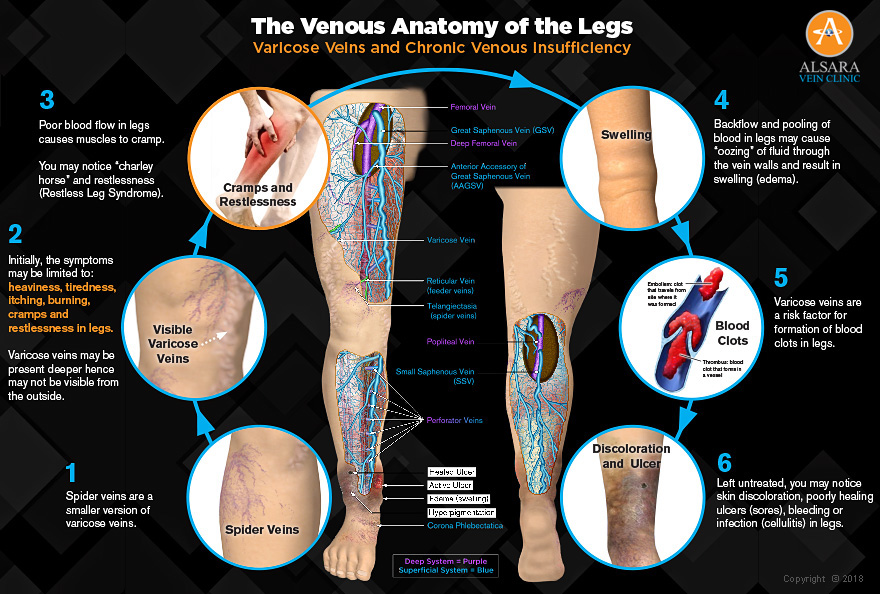
Although infrequent incidences of muscle spasms may not be anything to worry about, they are signs that the spasms might be more than a run-of-the-mill charley horse. Studies have shown that leg cramps at night are a very common manifestation of venous disease in the legs. Our veins are responsible for collecting de-oxygenated blood from the tissues and returning it to the heart and lungs, where the blood is replenished with oxygen and nutrients. Veins in the legs tend to fail more easily due to risk factors such as genetic predisposition, prolonged sitting or standing, pregnancies, and age. When some veins fail, the blood cannot flow through them effectively and starts pooling in the legs. In face of compromised blood flow, calf muscles are not able to function appropriately and cause cramps (charley horses) and restlessness (Restless Leg Syndrome).
WHAT IS IT?
WHO GETS THEM?
A "charley horse" is another term for a muscle spasm or cramp in the leg. While cramps can happen in any muscle, charley horse is most commonly noted in calf muscles and feet.
Anyone can develop a charley horse, however, according to the National Institute on Aging, not drinking enough water, poor muscle conditioning, and certain medications are factors that make people more susceptible to getting a charley horse as they age.
There are a few ways you can ease the pain from your charley horse. Drinking electrolytes and stretching can help to keep your muscles loose, as well as trying to take breaks from sitting for long periods of time. Applying an ice pack for 10-15 minutes following strenuous exercise can also calm down muscle tension.
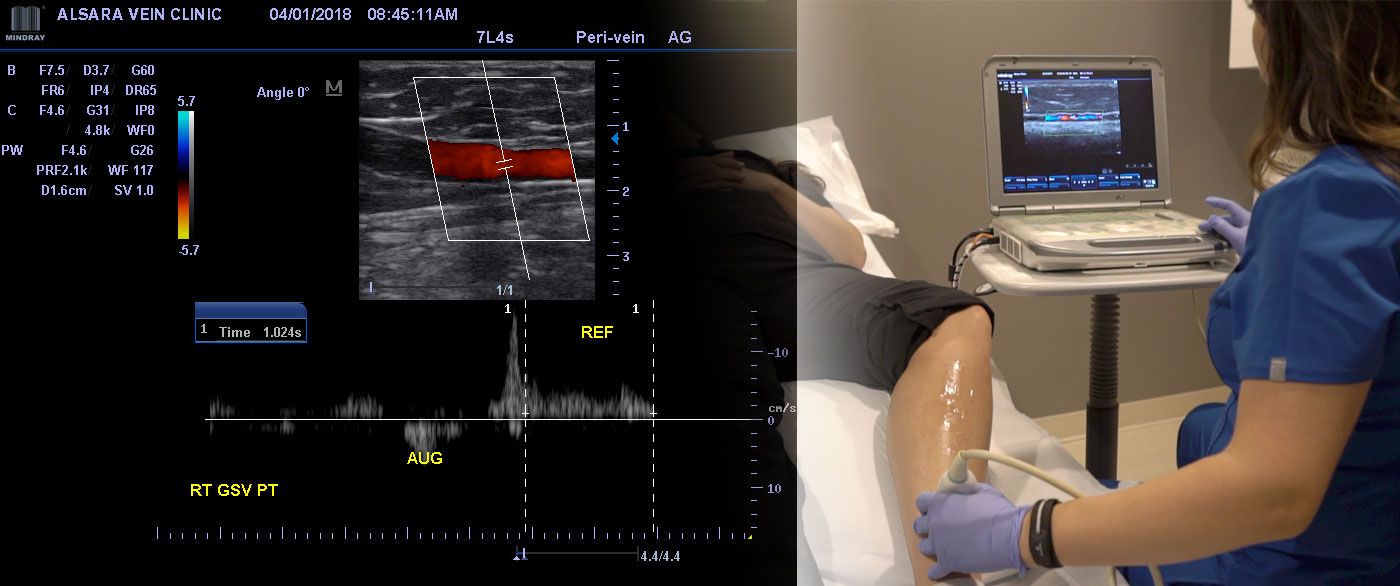
If you are experiencing muscle cramps regularly, it may be a sign of blood flow in your legs due to veins that have failed. Call us for a free consultation. Your Vein Specialist will ask you some questions and likely check the blood flow using ultrasound.
Remember that vein problems in the legs affect more than half of adults. In addition to leg cramps, you may notice heaviness in your legs, tiredness, itching, burning, restlessness, or leg swelling. The affected veins are typically deep inside the legs, hence you may not see them on the skin surface.
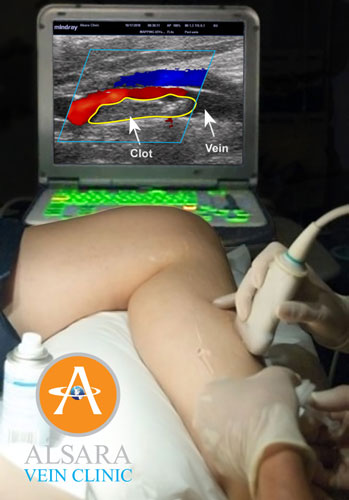
Left untreated, blood flow in the legs continues to worsen. Varicose veins and venous insufficiency may lead to blood clots, discoloration of the skin, sores that do not heal well, bleeding veins, and frequent skin infections.
Modern treatments are minimally invasive with minimal to no pain, no downtime, and almost all insurance companies offer coverage for symptomatic venous problems.
I cannot emphasize enough the seriousness of repetitive muscle cramps. One of our patients, Sandra Dyer, has graciously shared her story. She and her husband came to us looking for answers after three visits to the hospital for severe leg cramps.
Like most chronic conditions, left untreated, the diseased (varicose) veins continue to worsen and may cause other complications such as swelling, skin discoloration, blood clots, poorly healing sores, infection, or bleeding.
Using modern technology, we are now able to easily seal the diseased veins with help of endovenous laser ablation, allowing you to return to normal activities, without any downtime. Treatment of symptomatic venous disease is typically covered by most insurance companies including Medicare and Medicaid.
If “charley horses” are visiting you at night, call 816-396-0245 to get back in the saddle or schedule a Consultation today.
 Click to view large image
Click to view large image
 As I watched the colorful pictures on the screen, I thought of my mother, who passed away at a fairly young age after living with “heartburn” for years, that was treated with medications for indigestion. Being a woman and a diabetic are both major factors that confound the symptoms of heart disease. A slightly higher index of suspicion could have saved her life and one of the newer diagnostic tools such as the Coronary Calcium Scan could have kept her health in check.
As I watched the colorful pictures on the screen, I thought of my mother, who passed away at a fairly young age after living with “heartburn” for years, that was treated with medications for indigestion. Being a woman and a diabetic are both major factors that confound the symptoms of heart disease. A slightly higher index of suspicion could have saved her life and one of the newer diagnostic tools such as the Coronary Calcium Scan could have kept her health in check. Life is a beautiful journeyI witness the daily hopes and aspirations of numerous patients like this amazing woman who is 93 years “young”. Some have the usual symptoms of heaviness in the legs, cramps, restlessness, and swelling. Many others have lived long enough with vein problems in their legs and present with clots or sores in their legs. Hope tends to be contagious. Earlier this week, while treating a patient who came with a clot in her leg, I found out that her husband was also on my schedule. He has lived with swelling and sores in his legs for many years. She indicated with pride that, “I diagnosed his problem myself and told him to come and see you”. I won’t be surprised if he will soon be able to enjoy the full use of his legs without the constant fear of ongoing pain, infection, or even risk of amputation.
Life is a beautiful journeyI witness the daily hopes and aspirations of numerous patients like this amazing woman who is 93 years “young”. Some have the usual symptoms of heaviness in the legs, cramps, restlessness, and swelling. Many others have lived long enough with vein problems in their legs and present with clots or sores in their legs. Hope tends to be contagious. Earlier this week, while treating a patient who came with a clot in her leg, I found out that her husband was also on my schedule. He has lived with swelling and sores in his legs for many years. She indicated with pride that, “I diagnosed his problem myself and told him to come and see you”. I won’t be surprised if he will soon be able to enjoy the full use of his legs without the constant fear of ongoing pain, infection, or even risk of amputation.
 Dr. Gupta is certified by the American Board of Venous and Lymphatic Medicine. All clinical staff has specialized education and training for the management of venous diseases including all types of blood clots. Urgent Care centers, Primary Care Providers, Patients, and their relatives routinely call us for same-day appointments.
Dr. Gupta is certified by the American Board of Venous and Lymphatic Medicine. All clinical staff has specialized education and training for the management of venous diseases including all types of blood clots. Urgent Care centers, Primary Care Providers, Patients, and their relatives routinely call us for same-day appointments.

 There are also reports of blood clots in patients with COVID-19 who are at home and staying active. Swelling in the legs is the most common sign of blood clots. Some patients with COVID-19 develop a condition called “
There are also reports of blood clots in patients with COVID-19 who are at home and staying active. Swelling in the legs is the most common sign of blood clots. Some patients with COVID-19 develop a condition called “
 Click to view large image
Click to view large image Unable to move forward, blood begins to backtrack and pool in the legs causing the familiar symptoms of heaviness, achiness, and tiredness in legs, particularly in the evenings. Increased pressure on the vein walls makes them “gnarly” or varicose. Some veins that are close to the surface of the skin can be seen from the outside as ropy veins or spider veins.
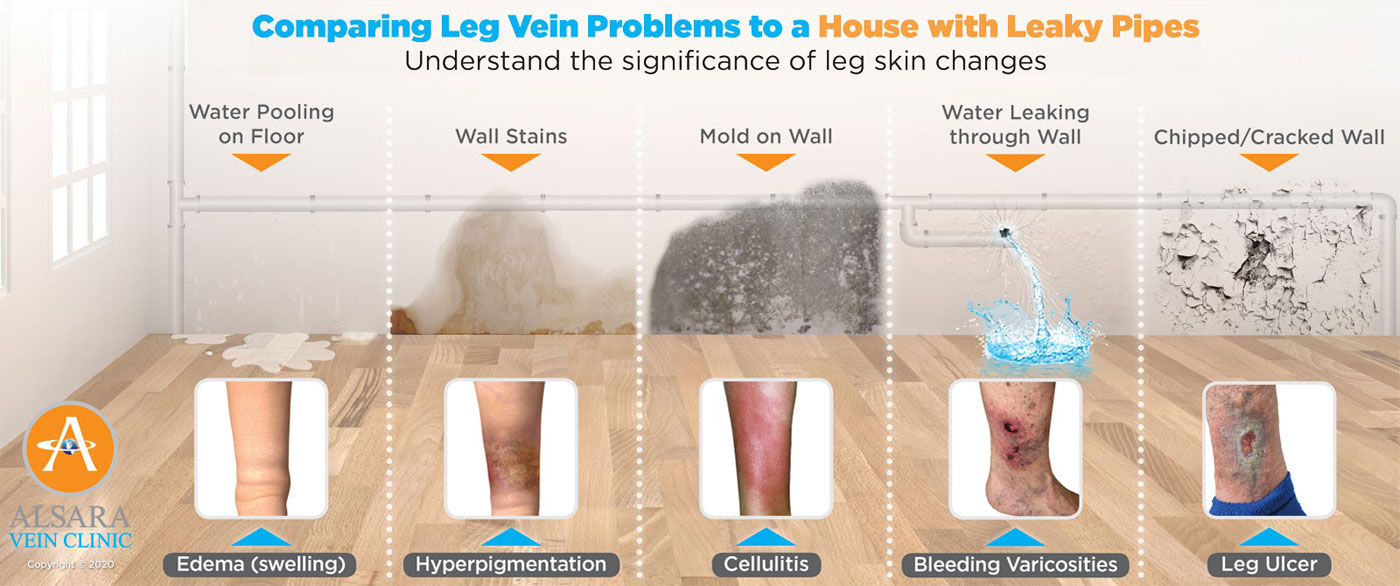
Unable to move forward, blood begins to backtrack and pool in the legs causing the familiar symptoms of heaviness, achiness, and tiredness in legs, particularly in the evenings. Increased pressure on the vein walls makes them “gnarly” or varicose. Some veins that are close to the surface of the skin can be seen from the outside as ropy veins or spider veins. Remember that the blood in veins is deoxygenated (has “low” oxygen content) and replete with waste products. This blood needs to be sent back to the heart where it can be enriched and put back in circulation. When there is an increased buildup of venous blood in the legs, patients may notice itching, burning, leg cramps (charley horses), and restlessness. Persistent stasis (pooling) causes hyperpigmentation (discoloration of the skin due to deposition of the hemosiderin pigment from the breakdown of red blood cells), cellulitis (skin infection), thrombosis (blood clots), and poorly healing ulcers (sores) in the legs. This is comparable to staining on the walls from leaky pipes, growth of mold, cracks in the walls, and eventually its breakdown.
Remember that the blood in veins is deoxygenated (has “low” oxygen content) and replete with waste products. This blood needs to be sent back to the heart where it can be enriched and put back in circulation. When there is an increased buildup of venous blood in the legs, patients may notice itching, burning, leg cramps (charley horses), and restlessness. Persistent stasis (pooling) causes hyperpigmentation (discoloration of the skin due to deposition of the hemosiderin pigment from the breakdown of red blood cells), cellulitis (skin infection), thrombosis (blood clots), and poorly healing ulcers (sores) in the legs. This is comparable to staining on the walls from leaky pipes, growth of mold, cracks in the walls, and eventually its breakdown.





 What made you choose us?
What made you choose us?

 The dreaded charley horse is reported to affect up to 60 percent of adults who have reported the presence of nocturnal leg cramps in the form of a painful spasm, tightening of calf muscles, and twinges. Numerous causes of charley horses have been described in the medical literature including muscle fatigue, dehydration, mineral deficiency, and poor circulation (venous insufficiency).
The dreaded charley horse is reported to affect up to 60 percent of adults who have reported the presence of nocturnal leg cramps in the form of a painful spasm, tightening of calf muscles, and twinges. Numerous causes of charley horses have been described in the medical literature including muscle fatigue, dehydration, mineral deficiency, and poor circulation (venous insufficiency). There are some easy ways to help prevent charley horses including staying hydrated, eating a balanced diet, avoiding excessive sugars and caffeine, and avoiding overexertion.
There are some easy ways to help prevent charley horses including staying hydrated, eating a balanced diet, avoiding excessive sugars and caffeine, and avoiding overexertion.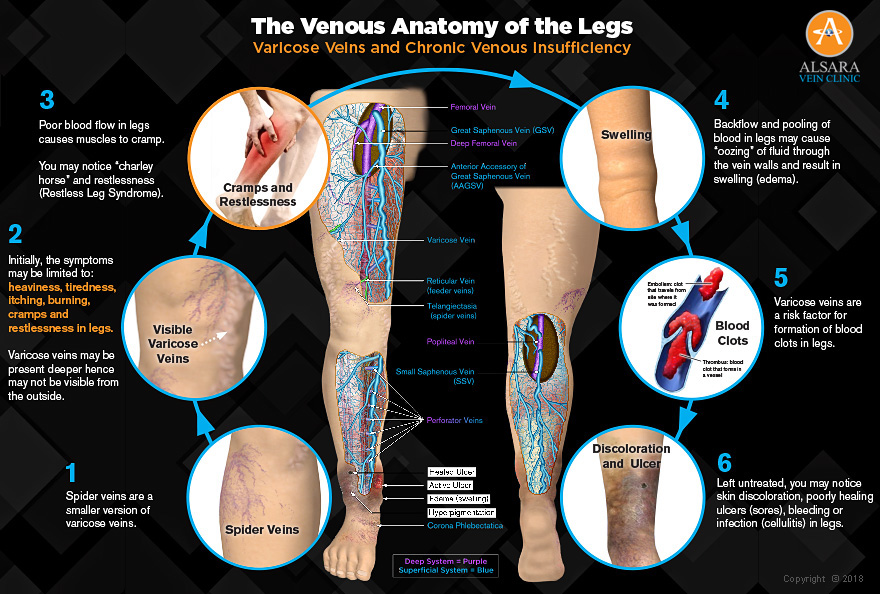 Click to view large image
Click to view large image


 I was born and raised in St. Joseph. I work at Missouri Western State University. I have two children and six grandchildren.
I was born and raised in St. Joseph. I work at Missouri Western State University. I have two children and six grandchildren.
 Varicose veins increase the risk of deep vein thrombosis (DVT) by five times
Varicose veins increase the risk of deep vein thrombosis (DVT) by five times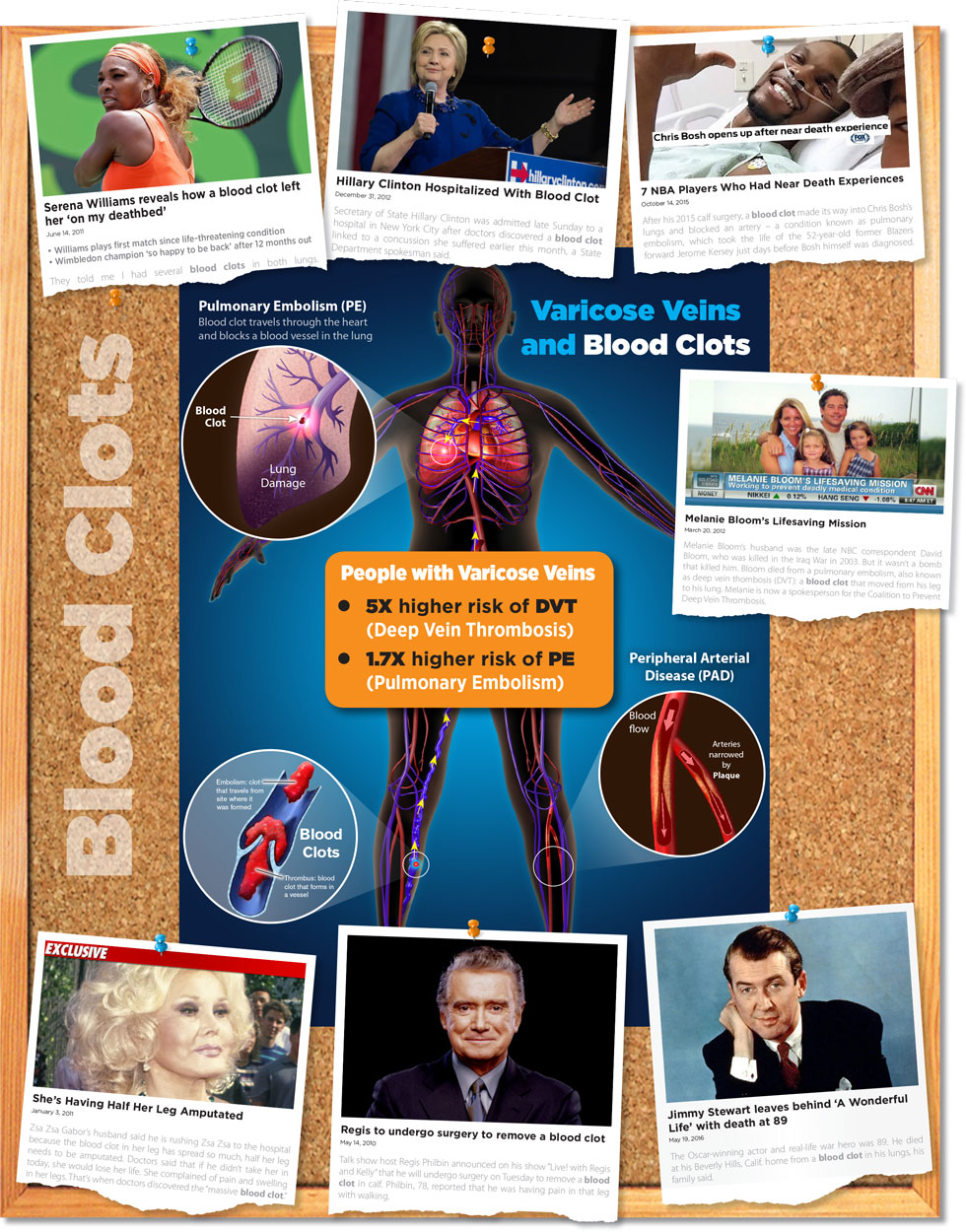

 Make sure you wear clothes that won’t trap heat. Always use sunblock (SPF 30 or above) not just on your legs, but also on your face and nose, where thinner skin is more prone to developing spider veins.
Make sure you wear clothes that won’t trap heat. Always use sunblock (SPF 30 or above) not just on your legs, but also on your face and nose, where thinner skin is more prone to developing spider veins.